Part of our ageing process is losing our teeth. Though this is an inevitable event when we reach our golden years, it’s still frustrating to think of the hassle and discomfort of being toothless.

Osteoporosis ICD-10 refers to a coding system in the medical field that is used to classify specific diagnoses, symptoms, and medical procedures for Osteoporosis.
Osteoporosis is one of the common musculoskeletal diseases among older adults, but women over the age of 50 are reported to be more at risk of the disease compared to men over 50. In fact, women who have undergone menopause usually feel the onset of Osteoporosis during their post-menopausal stage.
ICD-10-CM or known as the International Classification of Diseases, 10th revision, Clinical Modification is a coding system for certain diseases that helps experts in the medical field in diagnosing diseases and providing procedures for treatment. This coding system is approved and published by the World Health Organization (WHO).
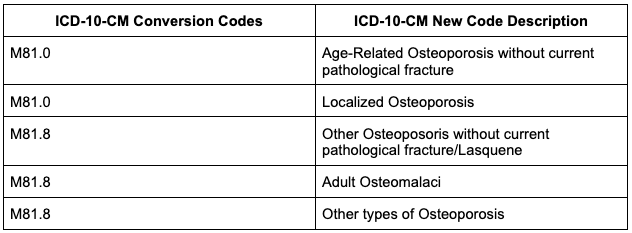
Generally, ICD-10 for Osteoporosis falls under the ICD codes M80 - M82, which includes Disorders in Bone Density and Structure. To give you an overview, here are the general ICD-10 codes for Osteoporosis:
Osteoporosis is a musculoskeletal disease that is characterized by weakness of the bones due to loss of bone density.
Bones are made of tissues, and as we age, these tissues replace old bones with new, strong ones. However, if you have Osteoporosis, more bones are being removed than it is replaced, which will then result in loss of bone density.
People with early-stage of Osteoporosis don’t usually feel its symptoms until it worsens. The primary symptom of Osteoporosis includes weakened bones, especially in the hips, wrists, and spine.
Age is one of the leading risk factors for Osteoporosis. That’s why if you would notice, most seniors aged 60 and above have weaker and more sensitive bones. Other risk factors of Osteoporosis include the following.
Osteoporosis does not show symptoms until it worsens, that’s why it’s important to get tested for Osteoporosis when you reach your 50s or 60s, especially if you are a woman. Though it’s a lot less common for men to get Osteoporosis, continuous monitoring, and regular check-up is still advised.
Once you are diagnosed with Osteoporosis, your doctor may recommend lifestyle changes and some medications depending on how severe your bone loss is.
Some lifestyle changes may include:
If you have severe bone density loss and that you have a high risk of bone fractures, lifestyle changes may not be enough to treat the disease. Therefore, your doctor may prescribe certain medications that may help slow down bone loss or rebuild bones that you lost.
These medications include
It is better to prevent Osteoporosis before it even starts. Experts recommend getting checked regularly to catch early signs of Osteoporosis and treat them before it gets worse. Also, below are several tips you should know to prevent Osteoporosis:
Final Word
Osteoporosis is one of the most common musculoskeletal diseases among older adults. Though there are treatments available to stop its progress and to rebuild lost bone density, it is still better to prevent the disease before it starts. Follow the tips mentioned above to maintain strong, dense, and healthy bones.
Part of our ageing process is losing our teeth. Though this is an inevitable event when we reach our golden years, it’s still frustrating to think of the hassle and discomfort of being toothless.
Getting regular exercise is one of the essential parts of healthy living for the young and old. However, as we age, many changes occur in our body including bone strength, muscle density, and flexibility.
Hearing loss refers to the condition where a person affected gradually loses his/her hearing. The normal hearing threshold of a person is 0-25 dB (decibels). This means that people whose hearing threshold is at more than 25 decibels have hearing loss.